Gut Microbiota: Key To Mental Health
The intestinal microbiota has been postulated as an excellent therapeutic target in the approach to different pathologies and health conditions. In this article we will focus on its relationship to mental health.
In 1683, Anton van Leeuwenhoek, spoke for the first time of some “animalcules” that he had seen in the gastrointestinal tract through the microscope. Today they are known as the gut microbiota.
The intestinal microbiota is defined as the set of microorganisms that inhabit the intestine in a symbiotic relationship with the host. It is estimated to be made up of 100 trillion microorganisms and the majority are found in the colon.
What is the gut microbiome?
We speak of the intestinal microbiome to refer to intestinal microorganisms, their genes and their active metabolites (substances produced by microorganisms and that impact the host’s organism).
The formation of the intestinal microbiota begins at conception and reaches maturity at 2 years of age. The perinatal period is critical: maternal habits during pregnancy, the type of delivery and the type of breastfeeding are the most influential factors.
Throughout adulthood there are different factors that can modify the microbiota. The most relevant are: diet, infections, use of antibiotics, stress, environmental pollution, excessive hygiene and consumption of toxic substances such as tobacco, alcohol or illegal drugs.
As a general rule, the diversity established in childhood returns when the factor that alters it is eliminated. However, modifications associated with the diet tend to keep it more stable.
The predominant phyla are: Firmicutes ( Lactobacillus and Clostridium ), Bacteroidetes ( Bacteroides and Prevotella ) and, to a lesser extent, Actinobacteria ( Bifidobacterium ). All 3 are essential in determining the states of eubiosis (healthy intestinal microbiota) and dysbiosis (alteration of the intestinal microbiota).
In 2011, the journal Nature published a study describing three Eubiosic enterotypes based on the variations of the three predominant phyla. However, a year later, the same magazine brought to light a new investigation that did not find the same conclusions.
Which functions has?
The intestinal microbiota has brain, digestive, immune, metabolic and endocrine functions, highlighting:
- Digestion.
- Synthesis of vitamin K, B5, B8 (biotin) and B9 (folic acid). It also produces B12 but this is not available to the body (it needs stomach acid to separate from its proteins and bind with intrinsic factor to form a complex absorbable by the small intestine).
- Maintenance of the integrity of the intestinal mucosa.
- Intestinal absorption of iron, calcium and magnesium.
- Regulation of amino acids such as tryptophan or glutamine.
- Modulation of the immune system.
- Reduction of glucose and cholesterol levels.
- Energy metabolism, regulation of lipogenesis and fatty acid oxidation.
- Synthesis of neurotransmitters.
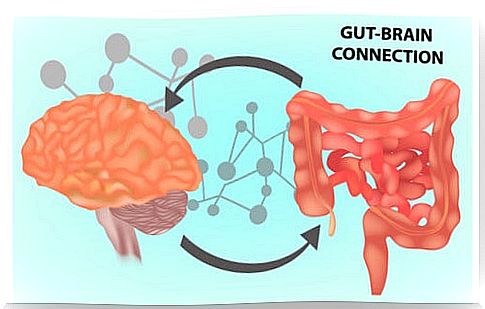
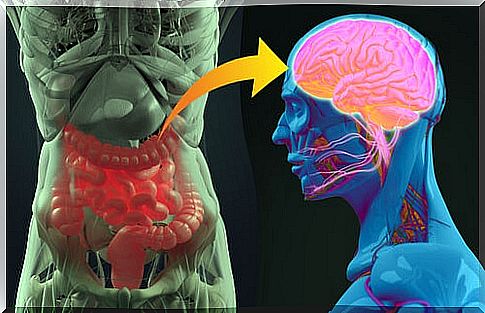
Gut microbiota – gut – brain axis
The intestinal microbiota is directly connected to the brain through the intestine, with numerous evidences of its influence on human behavior. This association is due to the existence of a multitude of neural connections between the two.
The vagus nerve
Here, the vagus nerve acquires special importance: it assumes a direct neural connection between the intestine and the brain. Thanks to it, the intestinal microbiota exerts a great influence on brain functions.
Neurotransmitters and hormones
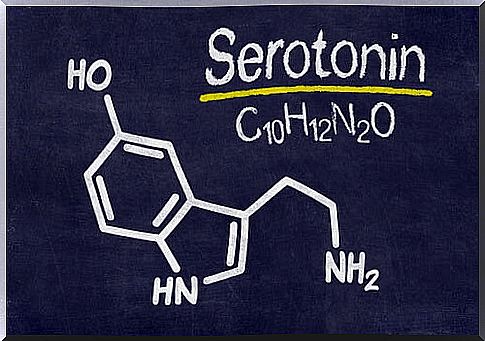
Part of the influence of the gut microbiota on the brain lies in its ability to produce neutransmitters (serotonin, dopamine, GABA, norepinephrine, acetylcholine, and cortisol) and amino acids (tryptophan) involved in brain function.
It should be noted that GABA and serotonin produced in the intestine cannot cross the blood-brain barrier. However, the short-chain fatty acids released by intestinal bacteria can do so and modulate GABA levels in the central nervous system. Furthermore, the tryptophan (serotonin precursor) produced by intestinal bacteria can also cross the blood-brain barrier.
Intestinal permeability
Dysbiosis involves an increase in intestinal permeability that increases the passage of toxic substances through the intestine. These substances stimulate the release of pro-inflammatory cytokines that, after reaching the brain through the vagus nerve, alter various brain functions.
The gut-brain connection is easy to understand if we observe that most mental disorders present with intestinal symptoms and that most people with digestive disorders suffer from a mental disorder such as depression or anxiety.
The gut microbiota is key in mental disorders
Current scientific evidence shows that the gut microbiota plays an important role in the development of mental disorders such as depression, anxiety, Alzheimer’s, Parkinson’s, obsessive compulsive disorder, eating disorders, autism spectrum disorders, multiple sclerosis, and epilepsy.
For example, dopamine, involved in the development of Parkinson’s, is lower in mice with an intestine free of microorganisms. If we go to autism spectrum disorders, we can see that 50% of those who suffer from it manifest gastrointestinal problems.
In addition, they have greater intestinal permeability and their microbiota is different from those free of the disease: less diversity, low levels of Bifidobacterium and excessive growth of Clostridium .
Another example is found in subjects with obsessive compulsive disorder who have a lower amount of GABA and serotonin. Both are produced by gut bacteria and modulation of the gut microbiota with probiotics has been shown to improve the disorder.
Constipation affects more than 80% of Parkinson’s patients and 30% of multiple sclerosis patients. In addition, malnutrition, Helicobacter Pylori infection, and bacterial overgrowth in the small intestine are common in the latter .
The role of probiotics in mental health
According to the WHO, probiotics are “live microorganisms that, administered in adequate amounts, confer a benefit to the health of those who take them.”
The term “psychobiotic” was described by a group of Irish scientists in 2013 and refers to any probiotic capable of exerting benefits on the brain. In this sense, it seems that Bifidobacterium Longum , Lactobacillus Ramnhosus and Bifidobacterium Infantis are its maximum representatives.
The bidirectional connection between the gut and the brain is unquestionable. More and more research supports the role of the gut microbiota in the development of mental disorders. The use of probiotics in the management of mental illness, although it requires further research, is supported by current evidence.